Bones are made up of living tissues that are constantly broken and replaced. Bones play an important role in more ways than one — they provide structure, protect your organs, anchor muscles, and store calcium. While peak bone mass is achieved during your 20’s and 30’s, you can take steps later in adulthood to protect bone health too.
Bones go through a state of constant renewal. In the case of an osteoporotic fracture, bone tissues do not get replaced by a new bone- the pace of new bone formation has significantly declined while on the other hand, loss of old bone occurs as usual.
In seniors, a bone-healthy diet plan, exercises, and medication can help to slow the rate of bone thinning and preserve muscle function.
Many studies say that osteoporosis is more likely to occur in older females than males, hence the fracture risk is higher in older females. Bone loss or porous bones is a major issue for females above the age of 30.
The onset of bone loss is earlier in women because they reach their peak bone mass in their early 20’s compared to the late ’20s in men. Insufficient calcium and vitamin D intake could also be a deterrent to healthy bone. This is the reason why doctors generally advise women in their thirties to take supplements for osteoporosis management.
Osteoporosis is a long-term condition, characterized by low bone mass and bone deterioration, leading to an increased risk of fracture. The most common fractures are:
- Wrist fracture
- A spinal fracture (vertebral fracture)
- Hip fracture
Contents
Osteoporosis Treatment
Osteoporosis is one of the most common bone diseases seen in human beings. It is characterized by a decrease in bone density that leads to fragile and weaker bones.
In a person with osteoporosis, the bone structure is compromised- the integrity of the bones is weakened and bone formation is adversely affected. This weakening results in higher bone fracture risks that are most often seen in the wrist and hip regions or spine collapses.
There are a number of medically approved ways to treat osteoporosis. Widely used drugs to treat osteoporosis are called bisphosphonates. These are generally made available in the form of:
- Fosamax (alendronate)
- Boniva (ibandronate)
- Actonel (risedronate)
By decreasing osteoclastic activity, bisphosphonate drugs decrease rates of bone resorption, resulting in an increase in bone mass when given to osteoporosis patients. There are two forms of bisphosphonate therapy which is commonly administered to osteoporosis patients-
- Oral bisphosphonates
- Intravenous bisphosphonates.
In recent years, research studies highlighting the benefits of CBD oil for osteoporosis are popularized, they are said to be beneficial in treating the symptoms of this bone disease. The studies show that CBD extract acts as a natural remedy in improving bone health. Additionally, CBD oil and other CBD products were found to improve the health of bone tissues, bone mass, and bone density of the weakened bone, promoting active living.
You may also like Can Osteoporosis Be Reversed?
What Are the High-Risk Factors for Osteoporosis?
Osteoporosis is a bone disorder that can occur in people of any age, race, and color. However, it is more common in adults, especially women. Here is the list of factors that may be a risk factor for osteoporosis:
- Family History: Having a family history of osteoporosis can increase your likelihood of developing osteoporosis.
- Lifestyle factors: Smokers and people who consume alcohol heavily. Also, a sedentary lifestyle where you get little or no exercise is detrimental to bone health.
- Being small-framed or thin: Thin people and those with small frames are more likely to develop osteoporosis.
- Inadequate Nutrients: A diet low in foods containing calcium and vitamin D.
- Certain medical conditions: Some medical conditions, such as hyperthyroidism or hyperparathyroidism, put you at greater risk for osteoporosis.
- Medications: Several medicines, such as corticosteroids used for long periods, cause bone thinning.
Other risk factors for osteoporosis may include:
- Being of European and Asian ancestry- the chances of osteoporosis is higher among people of these races.
- Restrictive dieting and eating disorders.
- Menopausal Woman: After menopause, estrogen levels, which protect women from bone loss dips. This leads to postmenopausal osteoporosis.
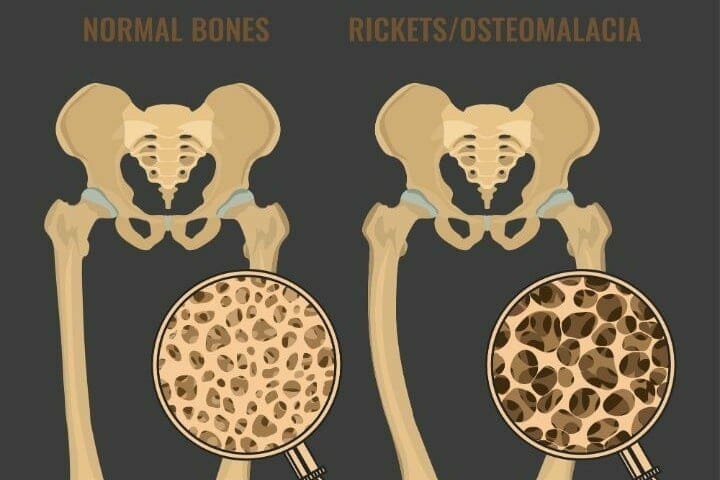
Osteoporosis and Osteomalacia:
It is important that you simply discern the difference between osteoporosis and osteomalacia before beginning treatment options.
We understand that the differences between Osteoporosis, osteoarthritis, and osteomalacia, could be confusing. So, we’ve given you an outline of the three:
Osteomalacia and osteoporosis make the bones weak. Whereas, osteoarthritis leads to the damage and tear of the joints.
Osteomalacia may be a curable bone disease. it’s the result of an imbalance between the demand and provide in bones for viosterol.
The symptoms are majorly bone pain and muscle weakness. The bone pain often increases during the night and is usually followed by tender bones.
Osteoporosis causes a decrease in bone density. In a person with osteoporosis, the body absorbs more bone tissue and doesn’t produce enough bone tissue to switch it.
This decreases their bone mass, resulting in lower bone strength and the next risk factor for fracture. The fracture risk is so high that even minor trauma sort of a coughing spasm can cause broken bones. This can be called a fragility fracture.
You may also like Intermittent Fasting and Osteoporosis
Diagnosing Osteoporosis in Elderly Adults
Broken bones can cause serious problems, especially for elderly adults who may have existing health complications. The hip may be a common problem area for elderly osteoporosis patients- hip fractures can cause a downward spiral of disability and loss of independence.
Osteoporosis is additionally common within the wrist and also the spine and elderly people may have a time managing daily chores like getting out of bed, brushing their teeth, and sitting up for extended periods.
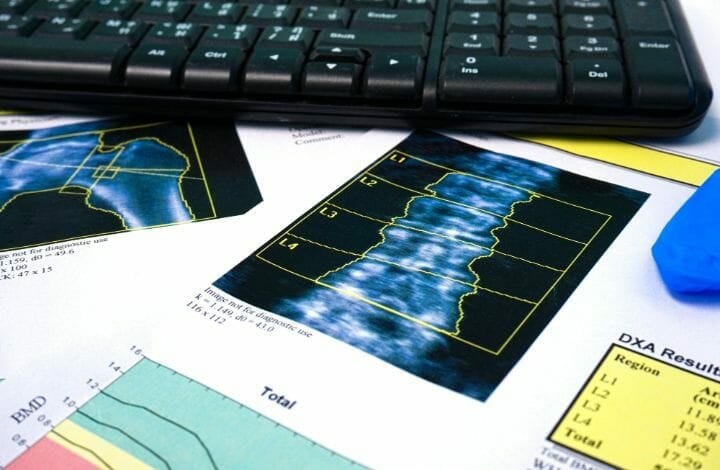
A Bone Mineral Density Test (BMD) which uses central Dual-Energy X-ray Absorptiometry (DXA) is the gold standard for identifying patients with osteoporosis. Your bone density can be measured by a machine that uses low levels of X-rays to determine the proportion of minerals in your bones.
The test is painless; all you have to do is lie down on a table as a scanner passes over your body. In most cases, only a few bones are checked, which are usually in the hip and spine.
DEXA Results:
Your results are often reported as a T-score- this compares your bone density to that of a healthy young woman. A T-score of −2.5 or lower means that you have osteoporosis.
What Are Your Treatment Options for Osteoporosis?
Osteoporosis treatment recommendations are often made on the estimate of your chances of breaking a bone in the next 10 years. The bone density test is a solid foundation to start on your treatment options.
If your risk for fracture risk and fragility fracture is not high, your treatment may not include medication. Rather, the treatment might be aimed at modifying risk factors for bone loss and falls.
Bisphosphonate
For people who are at an increased risk of fracture, the most widely prescribed osteoporosis medications are bisphosphonates. Examples of this medication include:
- Alendronate (Binosto, Fosamax)
- Risedronate (Actonel, Atelvia)
- Ibandronate (Boniva)
- Zoledronic acid (Reclast, Zometa)
Monoclonal Antibody Medications
Denosumab (Prolia, Xgeva) produces similar or better bone density results when compared to bisphosphonates. It also reduces the chance of all types of fractures. Denosumab is delivered via a shot under the skin every six months.
If you take denosumab, you might have to continue to do so indefinitely. Although very rare, recent research indicates there could be a high risk of spinal column fractures or a break or crack in the middle of the thighbone after you stop taking the drug.
A second rare complication is delayed healing of the jawbone (osteonecrosis of the jaw). This can occur after an invasive dental procedure such as tooth removal. We recommend that you undergo a dental examination before starting these medications. You should continue to invest time and effort in good dental habits and see your dentist regularly while on these medications. Make sure to inform your dentist that you’re taking these medications.
Hormone-related Therapy
The hormone estrogen helps to make and rebuild bones. A woman’s estrogen levels drop after menopause, and bone loss speeds up. Estrogen affects osteoporosis, which is why osteoporosis is most common among older women. But men get osteoporosis, too.
Estrogen can help maintain bone density, especially when you start taking it soon after menopause. However, estrogen therapy can increase the risk of blood clots, endometrial cancer, breast cancer, and heart disease. Therefore, estrogen is typically used for bone health in younger women or in women whose menopausal symptoms require treatment.
Raloxifene (Evista) mimics estrogen’s beneficial effects on bone density in postmenopausal women, without some of the risks associated with estrogen. Taking this drug can reduce the risk of some types of breast cancer. Hot flashes are a common side effect. Raloxifene may increase your risk of blood clots.
In men, osteoporosis might be linked with a gradual age-related decline in testosterone levels. Testosterone replacement therapy can help improve symptoms of low testosterone, but osteoporosis medications have been better studied in men to treat osteoporosis and thus are recommended alone or in addition to testosterone.
Now, along with supplements, osteoporosis medication, and treatments, weight-bearing exercises can improve bone health and quality of life. It is necessary to maintain the right bone mineral density with a nutritious, balanced diet.
You may also like Living Well with Osteoporosis
Bone-building Medications
If you can’t tolerate the more common treatments for osteoporosis — or if they don’t work well enough — your doctor might suggest trying:
- Teriparatide (Forteo): This powerful drug works like the parathyroid hormone and stimulates new bone growth. It’s administered daily by an injection under the skin. After two years of treatment with teriparatide, another osteoporosis drug is taken to ensure new bone growth.
- Abaloparatide (Tymlos): This is a drug similar to parathyroid hormone. You can take it for only two years. After two years, you will need to take another osteoporosis medication.
- Romosozumab (Evenity): This is the newest bone-building medication to treat osteoporosis. This drug is also given as an injection every month. It is limited to one year of treatment, followed by other osteoporosis medications.
Osteoporosis Pain Relief
Treatment for chronic pain in patients with osteoporosis is bisphosphonates, particularly alendronate, followed by denosumab, strontium ranelate, and teriparatide.
Can You Die from Osteoporosis?
Osteoporosis is often referred to as a ‘silent killer’. This is because many people do not realize that they have problems with bone mineral density and osteopenia until by accident.
It could be a fracture like a spinal fracture or any other kind of bone fracture after which the diagnosis tells them that they have a spongy bone disorder.
This bone disease is not fatal on its own but the effects and consequences are intense. Complications from any osteoporotic bone fracture can cause death.
Fracture in the thigh bone or a vertebral compression fracture can cause serious issues to overall health in the body. These issues make the management of osteoporosis in the elderly more complex.
If you are still wondering about the fatality of osteoporosis, know that death caused by osteoporosis is mostly due to the complications that arise after a hip fracture or spine fracture in the elderly.
Around 60 percent of elderly adults who have brittle bones and spongy bone disorder do not survive the complications caused by a hip fracture or a thigh bone fracture. Spinal fractures such as vertebral compression fractures are also quite untreatable.
Osteoporosis strips calcium from the skeleton and in advanced stages, collapses and bends the spins. It can lead to shattered hips, intense pain, and death after periods of being bedridden where the person most likely goes through a depressed state of mind.
According to statistics, almost 25% of people aged 60 and above who undergo a hip fracture die within a year from further complications.
The good news is that there are certain preventive measures you can take to prevent the onset of osteoporosis. It can also be treated with supplementation and a healthy diet plan. Weight-bearing exercise and Yoga are good for osteoporosis.
You may also like Aerobic Exercises for Seniors
Exercises for Osteoporosis
Osteoporosis management in older people (75 years and over) must focus on non-pharmacological and pharmacological interventions. The aim of treatment is to reduce morbidity and mortality associated with the first fracture and prevent subsequent fracture.
Yoga may also be an effective treatment for osteoporosis. Certain studies have found that practicing yoga for as little as eight to ten minutes daily can increase bone density.
Is Yoga Good for Osteoporosis and Osteopenia?
Yoga is a form of exercise that has been adopted worldwide due to its numerous benefits. Regularly practicing yoga can increase muscle strength, strengthen ligaments and tendons, and promote bone growth. Perform yoga asanas for osteoporosis after consulting with your doctor.
Stability and Balance Exercises
For seniors, especially those with osteoporosis, fall prevention is critical. Your body’s muscles have to work together to keep your body stable and upright. Balance-based activities like Tai Chi or even just standing on one leg are simple ways to maintain and improve your balance.
Here are a couple of easy-to-do stability exercises for seniors:
Foot Taps:
- Stand at the bottom-most step of a staircase.
- Raise your right foot to tap the step in front of you.
- Slowly return your leg back and place it on the floor.
- Repeat 15 to 20 taps on the right side.
- Repeat the same on the left leg.
Sit-to-Stands:
- Stand with your feet hip-width apart and with your back toward the seat of a sturdy chair.
- Sit back and slowly lower your hips onto the chair as gently as possible.
- Pause, and without moving your torso, push through your heels to stand up.
- Repeat 5 times.
Osteoporosis management in people aged 75 and over should be focused on a combination of non-pharmacological and pharmacological interventions. The aim of treatment is to reduce morbidity and mortality associated with the first fracture and prevent subsequent fracture.
You may also like Best Yoga Postures For Elderly
Management of Osteoporosis
Once osteoporosis has been diagnosed and the individual has been prescribed treatment for bone protection, there are important questions to consider before commencing:
- Has the patient been briefed about the goals of treatment?
- Does the patient agree to the treatment methods and process?
- What are the comorbidities or cultural aspects that may hinder the treatment?
- Can the patient swallow oral medicine and can they swallow safely?
- Can the patient maintain an upright posture for half an hour or so?
- Does the patient display signs of cognitive impairment?
- Does the patient manage their own medicines; if not, how would they keep track of their medications?
- Does the patient suffer from a renal impairment?
- Is the patient bedridden?
Preventing Spinal Fracture
Broken bones of the spine are common in people with osteoporosis and often go unnoticed until more serious problems occur. A compression fracture can be prevented by taking calcium supplements, getting more vitamin D, discarding habits like smoking and alcohol, exercising caution to prevent falls while moving around, and doing weight-bearing and balancing exercises. You can also take medications to halt or slow osteoporosis, mostly bisphosphonate drugs.
Elderly patients with osteoporotic compression fractures can be treated with TLSO bracing and rehabilitation. To facilitate progress, some patients may be treated in a less restrictive corset or abdominal binder, considering that their pain is under control.
You may also like
Preventing Falls in Elderly
Each year about one-third of all people over age 65 will fall. Many of these falls result in broken bones. Some common causes of falls include outdoor and indoor hazards. Certain lifestyle behaviors can also increase your chances of falling.
Outdoor Safety Tips
Here are some tips that can prevent you from falls when you are outside:
- Wear low-heeled shoes built with rubber soles for more solid footing, especially in winter.
- Use handrails while moving along steps and on escalators.
- If you find that the sidewalks are slippery, it is better to walk on the grass where you have more traction.
- It is prudent to carry a small bag of rock salt or kosher salt in your pocket or car during winters. You can then sprinkle the salt or kitty litter on sidewalks or streets that are slippery.
- Walk carefully on floors made of highly polished marble or tile as they can be very slippery.
- When floors have plastic or carpet runners in place, walk on them as much as possible.
- Declutter your porch, deck, walkways, and driveway from leaves, snow, trash, etc. Also, ensure regular maintenance.
- Cover porch steps with gritty, weather-proof paint and installs handrails on both sides of the steps leading to your door.
- If you are going out in the evening, turn on the light outside your front door before leaving so that you have outdoor light when you return after dark.
- Use a convenient, lightweight cross-body bag or fanny pack to store essentials so that you leave your hands free to support yourself in case you trip and fall.
- Invest in a good-quality walker or cane if needed.
- Contact community services that can provide help, such as 24-hour pharmacies and grocery stores that take orders by phone or internet and deliver so that you can avoid stepping out in poor conditions.
- Stop at curbs and assess the height before stepping up or down. Be careful at curbs that have been cut away to allow access for bikes or wheelchairs. The incline may lead to a fall.
- You can also consider wearing hip protectors or hip pads for added protection.
Indoor Safety Measures:
Following are tips to help prevent fall risk when you are inside your home:
- Keep items you use often within easy reach. This keeps you from having to bend down and stoop over.
- Use assistive devices if needed. You can use a long-handled grasping device to pick up items without bending down. Use a pushcart to move heavy items.
- If you must use a step stool, use a sturdy one with a handrail, wide steps, and non-slip legs.
- If you live alone, consider wearing a personal emergency response system (PERS) and/or a piece of medical alert jewelry. Also, consider buying a cordless telephone or cell phone that you can carry around with you so you can call for help if you fall.
You may also like
Bedroom
- Install light switches within reach of your bed.
- Place a night light within reach so that you can switch it on if you need to walk to the bathroom.
- Sit up slowly from sitting or lying down positions since moving quickly may cause dizziness.
- Keep a flashlight with fresh batteries beside your bed.
Bathrooms
- It is wise to install grab bars on the bathroom walls, beside the tub, shower, and toilet so that you can grasp onto it.
- Buy a non-skid rubber mat for the shower or tub. For more guidelines read how to make the shower floor less slippery.
- You can also use a plastic chair with a back and non-skid legs in the shower or tub.
- Use nonslip shower shoes.
Kitchen
- Use non-skid mats or rugs on the kitchen floor near the stove and sink.
- Clean up spills as soon as possible (in the kitchen and anywhere in the home).
Stairs
- Keep stairwells well-lit, with light switches at the top and the bottom.
- Install sturdy handrails on both sides.
- Mark the top and bottom steps with bright tape.
- You can also install slip-free strips and treads for stairs.
- Make sure carpeting is secure.
Floors
- Remove all loose wires, cords, and any rugs.
- Keep floors free of clutter and remove furniture with sharp corners.
- Be sure all carpets and area rugs have skid-proof backing or are tacked to the floor.
- Do not use slippery wax on bare floors.
- Keep furniture in a fixed place.
You may also like
In addition to indoor and outdoor hazards, certain lifestyle behaviors can increase the chances of a fall. Here are some lifestyle tips to help you:
- Minimize Alcohol: Keep track of your alcohol consumption. Alcohol slows reflexes and may cause confusion, dizziness, or disorientation. Excess alcohol can also cause bone loss.
- Mind Your Pace: If you are in a hurry, slow down. It is highly likely that you will trip and fall or head into an obstacle when you rush.
- Mindful of Your Surroundings: Stay alert and focused when in public places.
- Remember to wear appropriate shoes both indoors and out.
How to Boost Bone Health
Exercise and eat healthy at every age. A healthy diet includes having a well-balanced diet that contains the recommended amounts of calcium and vitamin D.
1. Exercise
Just 30 minutes of exercise each day can help strengthen bones and prevent osteoporosis. Weight-bearing exercises, such as yoga, tai chi, and even walking can stimulate bone cells to grow. Strength training builds muscles which also increases bone strength.
2. Eat a balanced diet
Dairy products fortified with Vitamin D, fish, and leafy green vegetables are all rich in calcium and Vitamin D, which have been shown to strengthen bones. In addition, there may be a link between Omega-3 fatty acids found in fish and flaxseed and bone health.
Blueberries might also strengthen bones. Eat at least five servings of fruits and vegetables daily, and three servings of low-fat dairy products like milk, cheese, and yogurt every day.
You may also like Pros and Cons of Weighted Vest for Osteoporosis
3. Take supplements
It’s challenging to get all the nutrients your body needs from the food you eat—especially if your appetite isn’t what it used to be. Calcium, Vitamin D, and Omega-3 supplements have all been shown to improve bone strength. Just be sure to check with your doctor to determine if any supplements you take might negatively impact the prescription medications you may be on.
4. Ensure that calcium and vitamin D is absorbed
Sunlight helps the body absorb vitamin D from the foods you eat. Experts recommend five to 10 minutes of sun exposure on the hands, arms, and face, two to three times a week, to help the body process the necessary vitamin D for bone health. Do not apply sunscreen while you are sitting out in the sun for this purpose.
5. Cut back on salty foods and caffeinated beverages
Foods that are high in salt or overly processed have been shown to prevent the body from absorbing calcium. Highly caffeinated beverages may have the same effect on your body. Limit intake of these foods for better bone health.
You may also like Apple Cider Vinegar and Osteoporosis
Conclusion
Evidence-based strategies should be the guiding principles for managing osteoporotic fracture risk in the elderly- take care to include weight-bearing exercise training, vitamin D and calcium supplementation, and the use of evidence-based anti-osteoporotic drugs a part of your regimen to manage this bone disease.
Do let us know what you think of the strategies mentioned above and how you find the information useful!