Contents
Bone is a mineralized connective tissue and its major components are a protein called collagen and calcium phosphate. While collagen is responsible for the softness of the tissue, calcium phosphate lends much-required bone strength.
Together both these elements make the bone flexible as well as hard. Our body needs another vitamin – vitamin D which helps us to absorb these two minerals. Our bones have a protective layer in terms of cortical bone. This cortical bone protects the inner cavity of the bones in the body.
From the beginning of life, our body generates new bone cells (bone formation, bone turnover, or bone resorption, increasing bone density/ bone mass) increasing bone strength, and removes old bone cells (resulting in low bone density/ decreased bone mass).
In the initial stages, osteoblasts secrete osteoid (Osteoid is the un-mineralized part of bone matrix that is formed before bone tissues mature) as several required proteins. At the onset of our life, the rate of bone formation/ bone resorption/ bone turnover far exceeds that of removal, and as a result, the overall volume of bones in our body increases and they become heavier and denser.
Normally, women attain peak bone mass in their early twenties whereas men attain peak bone mass in their late twenties. As our age increases, the rate of production of bone gradually starts to decrease. As a result, the difference between bone formation and removal slowly starts to decrease and can even be negative for some people after a certain age.
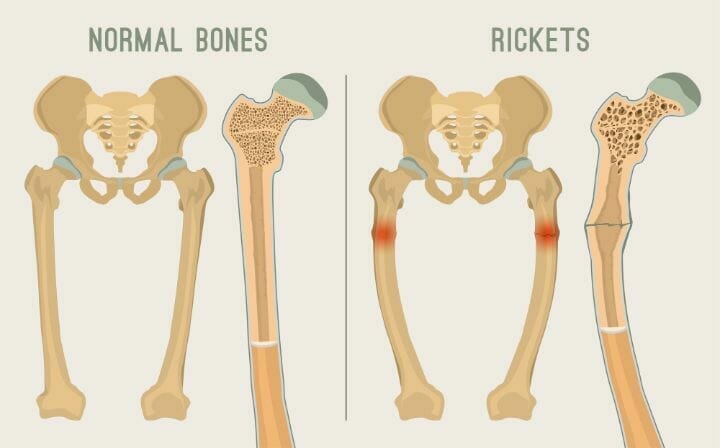
This is very common in post-menopausal women and in elderly men too, for whom the rate of bone degeneration is particularly high. Also, without the necessary vitamin D levels in our body, the bones become soft (this condition is called rickets in children) and lack the essential minerals required for bone health (i.e. lower bone mineral density/ decreased bone mass/ low bone density) as well as bone strength.
This is why bone health is particularly bad in many post-menopausal women and studies show that elderly women are more prone to metabolic bone diseases like Osteoporosis, Osteopenia, and Osteomalacia.
There are multiple conditions, like renal osteodystrophy, where the entire bone morphology is changed due to chronic kidney disease or CKD. The same disease (CKD) can give rise to secondary parathyroidism as well, which is caused by the excessive secretion of parathyroid hormone to counter hypocalcemia (low calcium levels).
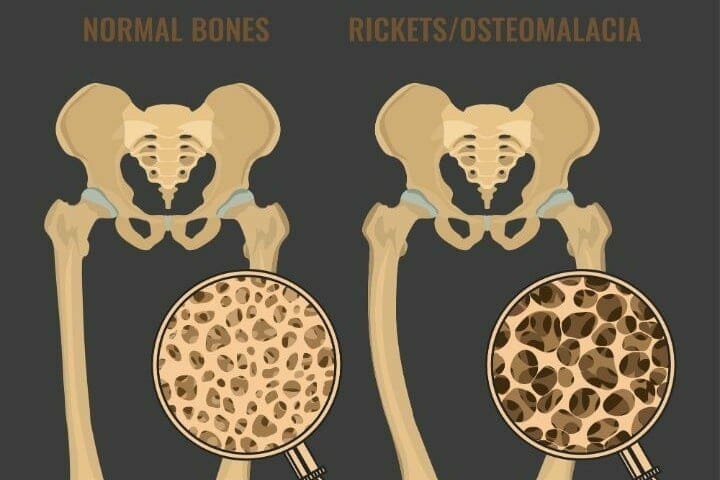
However, these are easily distinguished from osteoporosis and osteomalacia, which are often confused by a lot of people, because both of these result in loss of calcium in bone. But apart from that these two are very different in every other aspect and can be distinguished easily.
You may also like Does Smoking Cause Osteoporosis?
What is Osteomalacia?
Osteomalacia is a curable bone disease. It is the result of an imbalance between the demand and supply in bones for vitamin D. The symptoms are majorly bone pain and muscle weakness.
The bone pain often increases during the night and is sometimes followed by tender bones. It is easy to confuse osteomalacia with osteoarthritis, rheumatoid arthritis, or even neurosis and often it takes a considerable amount of time, even years, to diagnose osteomalacia.
Osteomalacia causes muscle weakness; the muscle weakness is most obvious in the pelvic region and most of the patients face challenges while climbing upstairs or sitting up from a supine position without the help of their hands. However, there would be no sign of neurological damage in the case of osteomalacia.
The weakness is a symptom of primary muscle disorder. The radiological signs/ Dexa scans/ bone density tests and even bone biopsy tests will only reveal a consistent lack of calcium. The results look like just how it would turn up when you do an examination for Osteoporosis.
However, Looser’s nodes, are very specific to osteomalacia, although it may not be present in each case of osteomalacia, and similar-looking lesions can arise in the case of Paget’s disease too.
Looser’s ends look like pathological fractures in the radiological images/ Dexa scans/ bone density tests, however are painless. Hence these are also called pseudo-fractures.
The most common and consistent biological change in the case of Osteomalacia is a rise in alkaline phosphate activity in blood.
Additionally, it can also be characterized by low serum phosphorus or low serum calcium levels. However, looking at elevated levels of alkaline phosphate in blood can be tricky, as there is no accepted normal level of alkaline phosphate in the blood.
Now, alkaline phosphate levels increase as you age. Elevated levels of alkaline phosphate can also be present because of other diseases, like Paget’s disease or chronic liver disease. This is why a vitamin D deficiency test is often considered to be the best factor to determine if a patient has osteomalacia.
In certain cases, osteomalacia can be healed by the introduction of vitamin D supplementation. However, the required level of vitamin D is high – above 150,000 i.u. per day. Hence a few scientists have suggested that osteomalacia can very well be a result of resistance (and consequently, a resultant higher demand for the same) to vitamin D in the body.
To combat the deficiency, once osteomalacia is detected, your doctor will likely suggest calcium supplements to be added to your diet. It is best that you continue taking the supplements at least for a couple of years, even if the symptoms are not apparent anymore.
Recurring cases of osteomalacia are common. This is why, in cases of elderly patients with osteomalacia, the doctor might suggest an oral intake of vitamin D (approximately 1000 i.u. per day) throughout their life span to prevent recurrence of the disease.
You may also like Apple Cider Vinegar and Osteoporosis
What is Osteoporosis?
Osteoporosis is a bone disease that occurs when the body loses too much bone, makes too little bone, or both.
The bone loss could be detected on radiographic diagrams/ Dexa scans, however, the images could not only be linked with osteoporosis (even there is a clear lack of serum calcium).
Osteomalacia can also show similar images. However, it is highly likely that the condition goes undetected as there can be no symptoms of osteoporosis at all for a long time. You may become aware of this condition only after breaking a healthy bone where you will likely get a Dexa scan.
Women are more prone to have Osteoporosis as compared to men, mostly as a result of low estrogen levels. One in every two women is likely to have Osteoporosis as compared to one in every four men. Also, senile osteoporosis is more common in elderly people, especially elderly women.
In some cases of osteoporosis, bone deformities or bone fractures (like femoral neck fracture) or an Osteoporotic fracture (like hip fracture, vertebral fracture, wrist fracture, femoral neck fracture, etc.) can be found.
Doctors have attributed these deformities and osteoporotic fractures to bone loss along with degradation in the quality of bone tissue. Interestingly, in elderly adults, there is no discernible change in the quality of bones and the scenario can only be explained by the degradation in the quality of the bone tissue.
The bone mineral density (BMD) test is the primary test used to identify osteoporosis and low bone mass.
The major issue in detecting osteoporosis lies in the fact that loss of bone tissue is common for many people when they age. And the doctors have not been able to ascertain whether this can unequivocally account for the problem of osteoporosis.
Sometimes, the loss of bone tissue may result in structural failure of the bone. Structural failure can be of different types and one can note that osteoporotic fractures in the spine and other long bones of the body are more frequent in the case of women as compared to men (above a certain age).
A few young individuals can also have the complication of low bone health or decreased bone density as compared to their age. The fundamental challenge, in this case, is not yet known very clearly, but these seem to be associated with some other issue as compared to osteoporosis.
Thin bones or low bone density for all ages (especially for young individuals) can be a result of either Cushing’s syndrome, thyrotoxicosis, or osteogenesis imperfecta and not necessarily osteoporosis.
However, the cumulative counts of all three are comparatively a lot rarer when compared with the thin bone scenario for elderly people (i.e. senile osteoporosis).
The treatment for the condition so far suggests that it cannot be corrected, at best it can be stopped.
There are a couple of modes of treatment available (estrogen therapy and calcium supplements), and both have their pros. However, it is difficult to choose one out of the two as a superior line of treatment.
Studies point out that the treatment of osteoporosis, in the future, can focus on reversing the loss of bone, however, when we can achieve it remains to be seen. For more interesting facts about osteoporosis, read here.
The differences between Osteoporosis and Osteomalacia can be summed as:
Osteomalacia Signs, Symptoms, and Treatment:
- Demineralization of bones
- Adults of both genders
- Weak muscles and fragile bones
- Vitamin D deficiency
- Vitamin D capsules/ injections are recommended treatment options
Osteoporosis Signs, Symptoms, and Treatment:
- A significant drop in bone mineral density- Majorly elderly women (>= 65 years of age, women are twice as likely as men).
- Curving of the back, higher bone fracture risk (like hip fracture risk/ vertebral fracture risk).
- Deficiency in calcium and phosphorus. Can happen because of drugs and alcohol consumption. Can be hereditary or linked to endocrinal diseases/ kidney diseases.
- Calcium supplements, healthy lifestyle to promote healthy bones are recommended as a treatment.
You may also like Living Well with Osteoporosis
Conclusion
Osteoporosis results in decreased bone mass whereas Osteomalacia results in softening of bones/rickets. While osteomalacia is caused by vitamin D deficiency, osteoporosis is caused by a deficiency of calcium and phosphorous.
Even the method of treatment is also significantly different for the conditions. Osteomalacia can be curable, whereas we don’t have a cure for osteoporosis yet, although there is ample information on the management of osteoporosis including weight-bearing exercises, Yoga, and Tai chi. Do reach out to a medical practitioner if you come across any of the symptoms.