is characterized by reduced and strength, resulting in increased susceptibility to . can cause intense that can affect a person’s quality of life. Fractures can increase your risk for disability or death.
This is associated with several risk factors. It is a chronic that poses a severe public health problem because of the high risk of low and non-traumatic fractures, especially to the vertebrae, hip, and forearm bones.
Growing evidence suggests that it can trigger or aggravate oral health problems such as , of the jaw, and and loss.
Contents
O
Various factors are responsible for the onset of in an individual. These factors may be age, race, lifestyle, genetic disposition, and certain medications, and treatments. Management of osteoporosis in the elderly and postmenopausal women can require extra care and effort.
Specific risk factors may include:
- Hormone levels in the body like estrogen levels, sex hormones, thyroid hormones, or adrenal glands.
- Dietary factors and lifestyle choices like , eating disorders and habits like a sedentary lifestyle, excessive alcohol consumption, and smoking can cause .
- Long-term usage of drugs and medicines like oral or injected corticosteroids may cause . These drugs directly interfere with the process of rebuilding and maintenance. is sometimes related to medications such as antiepileptics, antacids, chemotherapy, and immunosuppressants.
- The risk of osteoporosis is also increased in people suffering from medical problems like gastric issues like Celiac disease, inflammatory bowel disease, kidney or liver disease, cancer, lupus, and rheumatoid arthritis. Estrogen affects osteoporosis– it is a common cause of low bone health in women post-menopausal women.
Does Osteoporosis Affect Teeth and Nails?
Many studies and researches have been conducted over the last few years to determine the relationship between and teeth. The majority of them have studied the association between and , , eventual , and jawbone density.
The alveolar processes of the provide the basic bony framework for teeth support. The loss of systemic due to , especially in the oral cavity, can adversely affect the health of your teeth.
It has also been found that the decreased skeletal mass can be correlated with an increased risk of oral . It can result in a host system that is susceptible to infectious destruction of gum tissues. It can lead to .
causes changes in the mineral make-up of the alveolar and can lead to the progression of .
Loss of
A direct association between and has been established in recent years. Recent studies suggest a possible association between and among postmenopausal women and show a positive association between the two.
It has also been evaluated that has a negative impact on alveolar height in postmenopausal women. or other defects in children can rarely cause early exfoliation of deciduous or teeth.
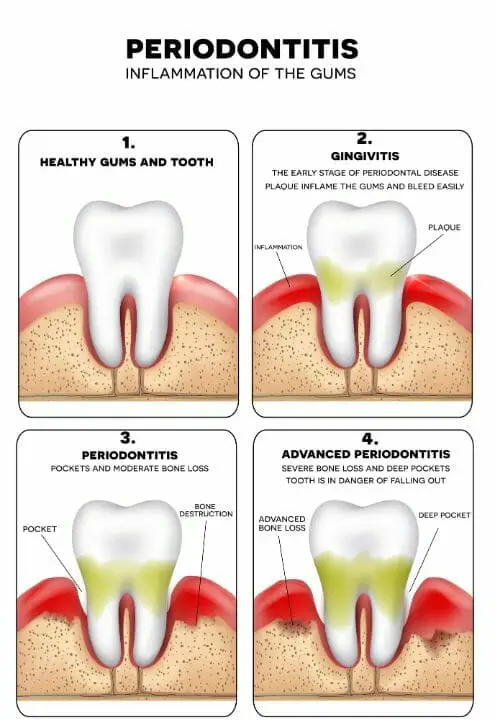
or P
and is a resorptive condition. is characterized by a reduction in leading to skeletal fragility and fragility fracture.
Periodontitis is characterized by resorption of the and is one of the significant causes of gum infection and in adults.
As loss of alveolar is a result of , severe can be a triggering factor in the case of gum and periodontal tissue decay. It is often seen that the breakdown of periodontal tissue may be related to systemic diseases, including .
Also, many studies have proposed and proved the role of in the onset and progression of periodontitis () and . It can also be used vice versa; can be an indicator of .
Loss of Bone Mass and Bone Density
also results in the loss of throughout the body, including the maxilla and the mandible (upper and lower jawbones).
The resulting low and in the jawbones leads to increased porosity, changes in trabecular pattern, and faster alveolar resorption.
It leads to invasion by periodontal bacteria and there is a high-risk for infection. Some systemic factors like interleukins and cytokines which affect remodeling may also lead to changes in the local ‘s response to periodontal infection.
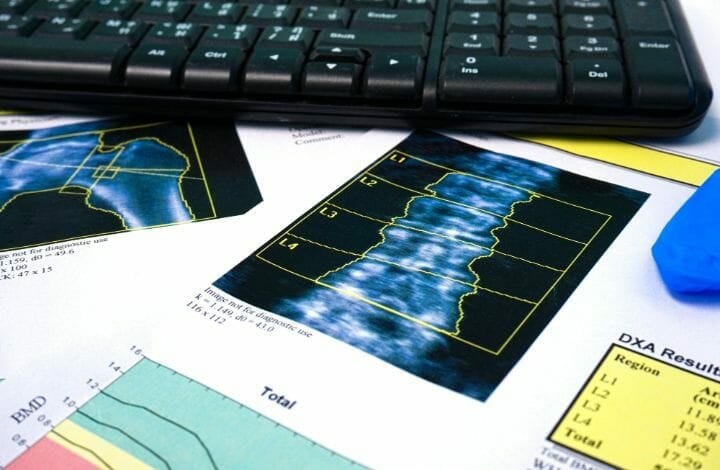
Cytokines are biochemicals produced by osteoblasts or -forming cells that have a vital role in remodeling and balance. The best way to check is a called DEXA (Dual-energy x-ray absorptiometry).
The dental and oral effects of generally affect more women than men. It holds for women who are already in the menopausal phase (unless they regularly use a therapy designed to replace lost hormones and balance them.)
It should also be taken into account that even if a person has no teeth and does not use dentures, can still show detrimental effects on dental and oral health. weakness and loss can damage the bony ridges that hold dentures in the proper position.
It results in ill-fitting dentures. Research shows that osteoporosis patients are at risk of requiring new dentures more often than those with strong, healthy bones.
Women who have are most likely to experience difficulties linked to poor-fitting dentures or loss of dentures. The results of oral and dental surgical procedures are also not as effective for women with .
You may also like Difference Between Osteoporosis and Osteomalacia
Treatment of Offect on Oral Health
Apart from the effects of on oral health, bisphosphonate, which is used to treat , causes of the jaws. It is a significant concern to a dentist or oral surgeon. The exact mechanisms by which the drugs act or cause necrosis of the jaws remains unclear.
The connection between of the jaw and bisphosphonate use has not been determined yet. Hence, any form of invasive dental treatment like , for example, should be performed with utmost care in patients taking bisphosphonates.
Medical data suggests that people who take bisphosphonates require special attention during dental treatment. Special care should be taken while placing dental implants or performing a , due to a concerning occurrence of bisphosphonate-related of the (BRONJ) or .
and the Health of Your Nails
Chipping nails could be a sign of poor . If it occurs frequently, it could indicate that the bones are just as brittle. A few studies suggest that people who have low collagen levels, which is a type of strengthening protein, in their nails don’t have enough in the bones, either.
Meanwhile, weak nails that often break and chip or vertical nail ridges show that their body lacks -building . Bones and nails are partly made up of a protein called collagen, which gives them structure and strength.
As people age, the collagen in the body deteriorates, leading to a reduction in and mineral density. This decrease in collagen and reduction in might be due to .
density tests measure the density of minerals like in bones. Low and are associated with weaker bones and the for the development of . Low levels of collagen can also lead to heart disease, autoimmune diseases like rheumatoid arthritis, and reduced hair growth.
You may also like CBD Oil for Osteoporosis – Benefits and Options
Osteoporosis: Caring for Oral Health and Nails
Prevention of starts with consuming calcium-rich, getting enough , and performing exercises-isometric exercises for osteoporosis, coupled with yoga and weight-bearing exercises are beneficial.
- Basic lifestyle changes can ensure a higher . Prevention measures are especially relevant to women, who are at a higher risk of this . A healthy diet plan for prevention and regular exercise are recommended.
- The best way to correct and prevent oral health problems is to avoid delaying or postponing dental treatments. Regular dental visits are essential in fixing issues in oral and dental health caused by weak bones. A healthy lifestyle is necessary for strengthening and maintaining good healthy as well as .
- Practical tips in optimizing and include consuming a well-balanced diet containing high amounts of and and performing regular physical activities. Increased consumption of calcium-rich such as milk, yogurt, cottage cheese, kale, broccoli, and sardines are beneficial.
- Supplements for can also be taken to prevent . However, older people must consume and supplements with caution. According to the American Dietetic Association, “The recommended are not more than 2.5 grams a day and not more than for , 1,000 per day. Consuming more than the recommended levels can prove to be toxic to the kidneys, liver, or heart.”
- The best exercises for strengthening bones are jogging, weight training, and aerobics, dancing and walking. Yoga for is gaining popularity as an effective way to manage the effects of .
- Immediately report problems to your dental office related to , ill-fitting or loose dentures, and / . It is also important that you maintain oral hygiene at home too. As age increases, it may become difficult to do so. Therefore older individuals must use dental floss that has a handle and a toothbrush with a bigger handle. Another trick is to attach a rubber ball around the handle of the toothbrush. They can also simply switch to an automatic toothbrush.
Collagen For Osteoporosis:
Consuming collagen supplements may help reduce the risk of disorders like . They have the potential to help increase and lower levels of proteins in the blood that stimulate breakdown.
Various studies have demonstrated that collagen supplements may have specific effects in the body that help inhibit breakdown, leading to . Collagen and calcium supplementation can also improve the health of skin, nails, and hair.
There are various studies that strongly suggest that collagen can strengthen . Collagen supplementation is also known to stimulate differentiation of the -building cells (osteoblasts) to produce a new collagen matrix.
Collagen supplementations also enhance the existing -collagen matrix while reducing the activity of the -breakdown cells, also called osteoclasts. Another bonus of supplementing with collagen is an increase in skin hydration and elasticity to reduce wrinkles. Collagen will help maintain youthful and radiant skin as well as . Collagen is a great supplement to combat too.
results from a gross imbalance in the rates of formation and resorption that cause bones to lose mineral mass. It most often affects middle-aged and elderly people, the same group of the population with the highest risk of chronic () and .
Evidence suggests that there is an association between periodontitis and , but there is hardly any awareness about the extent to which dental health can be impacted.
Many more studies and awareness programs are required to assess the role of in various oral conditions, to demonstrate the clinical effects of therapies on oral health and nails. It is vital to throw light on the fact that dental and dermatological examinations are of huge value for initial screening for signs of .
If you found the information helpful, do let us know in the comments below!