is a condition that affects a vast number of people around the globe, especially females. causes loss of and . This leads to decreased , raising your .
Bones are living tissues that are constantly remodeled which means they are broken down continuously and replaced. This is termed , and it determines .
the new cannot keep up with the loss of . This makes the person more susceptible to fractures.
In fact, in severe cases, the bones become so brittle that a slight fall or even a violent cough can cause .
generally remains asymptomatic until the first signs of (following minor accidents or injuries), particularly in the case of (mostly occurs to the ). The insides of your have a honeycomb structure with many small spaces.
In a person with , these small spaces increase in size, resulting in reduced and .
Contents
?
is generally classified as and .
Primary Osteoporosis of two types:
Type I O(P):
As the name suggests, this generally develops after menopause. Estrogen affects osteoporosis– when estrogen levels drop precipitously, hormonal changes lead to , usually in the trabecular (spongy) inside the hard cortical .
Type II O (S):
Senile osteoporosis is commonly found in people in their seventies and involves a thinning of both the trabecular (spongy) and cortical (hard) .
can cause a notable decline in . This is due to an imbalance between and . and are the essential components of .
It is defined as that results from specific, well-defined clinical disorders. Secondary osteoporosis can be reversed.
You might also like Best Weighted Vest for Osteoporosis
What Are the Causes of Senile Osteoporosis?
is an age-related disorder found mostly in people of seventy years of age, leading to the attenuation of both the and .
The is affected badly because it is lighter and more porous than compact . makes up about 20 percent of the human skeleton and provides structural support and flexibility. It provides more surface area for and is more metabolically active.
is a geriatric disorder -an imbalance in that occurs as people age plays a major role in the development of . The maturing cortical and trabecular bones, in particular, cause a reduction in the of the elderly.
Risk Factors for S
The for consists of age, race, lifestyle choices, genetic diseases, and certain medical treatments.
When it comes to impact, a is more likely to be affected by this disease when compared to adult men.
The risk factors may include the hormone levels in the body (sex hormones, thyroid hormones, or adrenal glands), dietary factors, and lifestyle choices (low diet, eating disorders, or recent gastrointestinal surgery).
A sedentary lifestyle, excessive alcohol consumption, and tobacco use can also elevate the risk of . Long-term usage of drugs and medicines like oral or injected corticosteroids may also cause .
These drugs directly interfere with the process of rebuilding and maintenance. is sometimes related to medications such as antiepileptics, antacids, chemotherapy, and immunosuppressants.
Medical Conditions That Aggravate Osteoporosis:
The risk of osteoporosis is high among people suffering from medical conditions like Celiac disease and inflammatory bowel disease, kidney or liver disease, cancer, lupus, and rheumatoid arthritis.
Some studies reveal strong evidence that the development of is related to a deficiency of zinc in the body. Zinc deficiency plays a role in the pathogenesis of .
Zinc deficiency can lead to increased endogenous heparin in the body. This leads to , making bones more fragile. These factors are known to enhance the pathogenetic process attached to as they elevate the action of the .
Research reveals that stromal cells differentiate into more adipocytes as age increases rather than going through . (Osteoblasts are responsible for ).
These stromal cells undergo aging. Eventually, there is a significant reduction in leading to .
A low diet and a decrease in the absorption of also contribute to a diagnosis of . As people age, the collagen in the body deteriorates, leading to a reduction in and .
This decrease in collagen and reduction in might be a cause of . As density measures the density of minerals like in bones, a and are associated with and the likely development of and fractures.
Reduction in collagen can also lead to , autoimmune diseases like rheumatoid arthritis, and reduced hair growth.
You might also like Pros and Cons of Weighted Vest for Osteoporosis
What Are the Complications Caused by
Vertebral compression (VCFs) is the fracture of the bones in the back. It can cause long-term complications, including curvature of the spine (kyphosis), intense back and joint pain. VCFs can also increase deficits in physical, psychological/social functioning.
Further complications include:
- Reduced range of motion
- Collapsed lung or pneumonia
- Compression of abdominal organs leading to decreased appetite and constipation
- Deep venous thrombosis
- Progressive muscle weakness
- Increased risk of repeated vertebral fractures
These are some of the consequences of VCFs. Advanced stages of senile osteoporosis can lead to death.
Colles’ Fracture
Further complications include:
- Persistent neuropathies of nerves in the arm
- Radiocarpal or radio-ulnar arthrosis
- Tendon ruptures
- Associated injuries
- Stiffness in fingers
- Shoulder-hand syndrome
Hip Fracture
Osteoporosis can cause pain in the hips. In the advanced stages, there are chances of hip fracture and about half of the people who suffer from a remain unable to fully regain their mobility.
If a keeps you immobile for a long time, bedsores and risk of urinary tract infections are normal.
Further complications include:
- Blood clots in your legs or lungs
- Pneumonia
- Further loss of muscle mass, increasing your risk of falls and injury
Additionally, people who’ve had a are at increased risk of weakened bones and further falls — which means a significantly higher risk of having another .
Hip and vertebral are associated with significantly higher mortality rates. There is no proven solution to improving survival in to date.
The independent role of fractures versus other factors, including functional status, comorbidities, capacity for independent living, etc., in increased mortality rates is uncertain.
Timely treatment of , with a diet plan for osteoporosis for patients who already suffered from a , reduces morbidity and may translate into better chances of living well with osteoporosis.
You might also like CBD Oil for Osteoporosis – Benefits and Options
Prevention and Treatment of S
It is important to evaluate the risks for poor at all ages. Those in greatest need should receive a full assessment of and fragility .
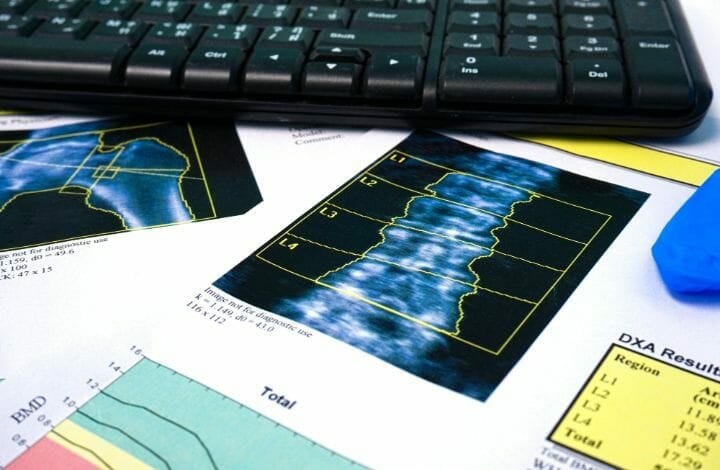
The best way to check is a scan called DEXA (Dual-energy x-ray absorptiometry). The Assessment Tool (FRAX) is a tool that can give an estimate of the probability of a major in the future.
This algorithm is designed for primary care. Along with age and genetics, is the next major determinant of .
Individuals with a low trauma or low for their age should get themselves checked to find out the underlying causes of . Secondary causes account for up to 40% of cases of in women and 60% in men.
The goal of management is to reduce the future risk of . Lifestyle modification includes measures to reduce falls risk and such as exercise, adequate dietary , and avoidance of smoking, and excessive alcohol consumption.
Good nutrition and regular exercise are key to prevention. The elderly at risk of should reduce alcohol consumption and smoking.
Now, osteoporosis in the elderly can give rise to a host of oral health issues. Regular dental visits are essential in fixing these dental concerns caused by weak bones.
Foods for B
Consume a well-balanced diet containing high amounts of and . -rich foods include milk, yogurt, cottage cheese, kale, broccoli, and sardines.
Supplements for osteoporosis can also be taken to prevent deficiency. However, older people must consume C and V supplements with caution. The best exercises for strengthening bones are jogging, weight-bearing exercises, aerobics, dancing, and walking.
Treatment for
Many drugs can reduce from worsening. Alendronate and risedronate, consumed once a week provide a significant reduction in further . Denosumab is approved for in women.
Strontium ranelate also has been shown to reduce significantly in postmenopausal women. Certain genetic recombination therapies involving and genetic enzymes have also been suggested to promote .
When it comes to the management of osteoporosis in the elderly, findings reveal an acute loss of , followed by a more progressive decline in . A significant increase in leads to an initial fall in . With increasing age, there is also a significant reduction in .
New potential treatments, including therapeutic approaches to in elderly people focusing on the pathophysiology and possible reversal of the adipogenic shift in , must be popularised.