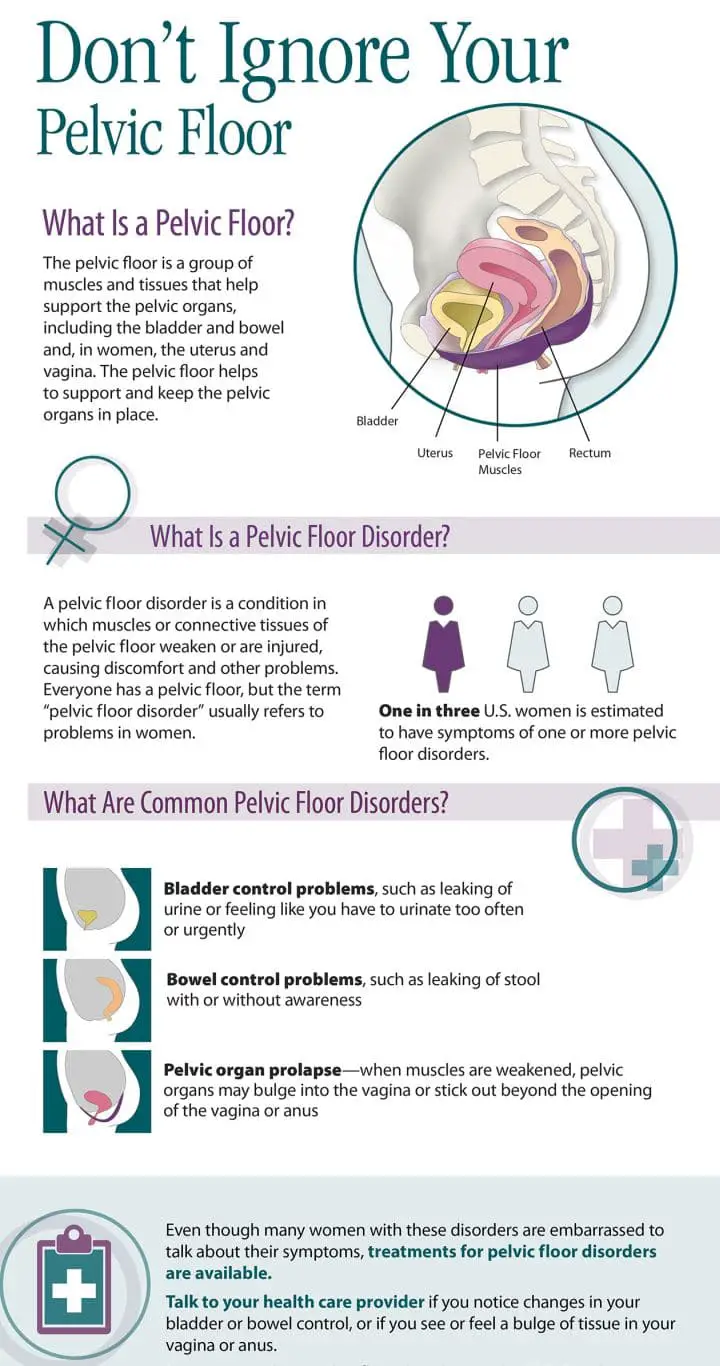
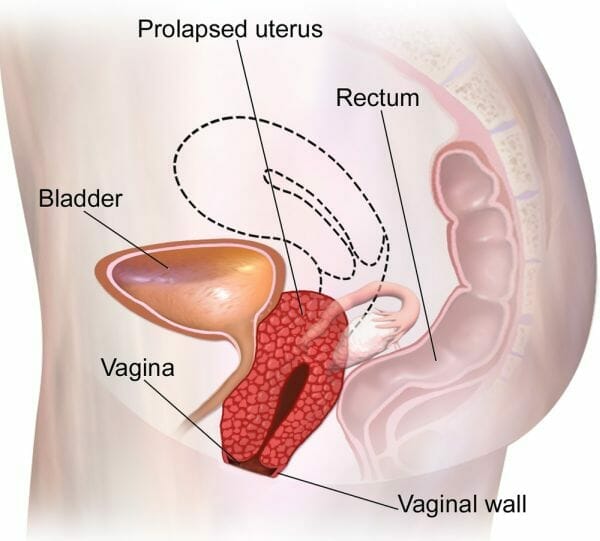
Pelvic organ prolapse (POP) is a condition that causes loosening of the vaginal or rectal wall leading to protrusion of bladder, uterus, small or large bowels from vagina or anus. It is commonly caused due to growing age, normal delivery, and obesity. It damages the molecular structure of the body causing loss of anatomical support leading the organs to fall. They are classified as per loosening of anterior, posterior, and apical and are graded from stage I to IV.
Contents
Symptoms of Pelvic Organ Prolapse
The patient most commonly complains of bearing down sensation. Other symptoms of POP include:
- feels a lump coming out of the rectum or vagina
- Abdominal and back pain
- bulging of the vagina or the bladder
- Irregular bowel movements
- Urinary tract infection
- Gastrointestinal infection
- Painful intercourse
The symptoms rarely result in mortality but they rather affect patients, quality of life.
Diagnosis
- Patient history: A thorough history taking is an important step in diagnosing. Prolapse-related symptoms and risk factors associated with it are diagnosed through history and this helps in determining the treatment plan.
- Physical examination: Pelvic examination by a physician is typically used to diagnose prolapse. Abdominal pressure is assessed while relaxing in a supine position. The prolapse wall involved (anterior, posterior, and apical) is evaluated by examining the vagina. Also, the degree of prolapse is determined when the patient is in a standing position.
- Imaging: It is useful in identifying the wall involved especially for patients showing no signs in the physical examination but have bulging symptoms.
You may also like How to Sleep With Lower Back Pain and Sciatica?
Treatment
Treatment is required for patients showing symptoms like bulging of pelvic organs, urinary, bowel, or sexual dysfunction. Asymptomatic usually do not require treatment. Treatment can be conservative or surgical depending on patient choice, age, stage of prolapse, and general health of the patient1.
Treatment for prolapse includes:
- Pelvic floor muscle exercise/Kegel exercises: Surveys and analysis on muscle strengthening have shown a positive effect on prolapse stages and symptoms.
- Physiotherapy: Regular physiotherapy help in strengthening pelvic muscles and prevent further loosening of organs from the pelvic wall.
- Hormonal therapy: As menopause and hormonal imbalances are risk factors of prolapse, hormonal therapy can be useful for its treatment. The use of topical estrogen hormone helps in relieving prolapse.
- Surgical treatment: Surgical treatment is either reconstructive (for symptomatic patients) or obliterative (for older age, patients who can’t tolerate extensive process). anti-incontinence procedures and hysterectomy are also treatment options. The abdominal surgical route is usually taken for patients with anterior or posterior prolapse but it has a high recurrence rate of 30%. Subtotal hysterectomy, para vaginal repair, and surgical mesh are procedures that reduce recurrence.
- Insertion of pessaries: They are the best conservative treatment option. Pessaries are indicated by over 85% of gynecologists and almost 98% of urologists. It is a non-invasive treatment option and helps in restoring the anatomical structure. There are two types of pessaries internal and external. Both functions to support the anatomical structure and prevent falling of organs from the vagina. Femicushion is the best-used pessary to treat pelvic organ prolapse.
You may also like Best Chair for Hip Replacement Patients
Femicushion for Prolapse Support
Femicushion is an external pessary developed to overcome the disadvantages of internal pessaries at the same time giving equal support. Below are some of the benefits of Femicushion2:
- It benefits patients who are not advised for surgeries or want to delay surgery.
- It Improves the quality of life by allowing the patient to perform day to day activities. Studies have shown a reduction in prolapse symptoms within three months.
- It keeps the prolapse above the vaginal introitus level and prevents its falling. Women with stage 2 or beyond prolapse have found this to be a helpful device.
- A decrease in prolapse degree has also found in few studies due to reflex contraction of femicushion and absence of protruding lump from the vagina while performing daily activities.
No products found.
How Does Femicushion Work?
It forms the base of the vaginal wall supporting the pelvis muscle. It also elevates the bladder to its anatomical position. They provide support blocking the opening and thereby preventing falling of the lump from the vagina. It also causes reflex contraction of the muscles thereby reducing the degree of prolapse.
Advantages of using Femicushion
- Easy placement
- Avoids complication of vaginal fistulas or ulcer
- An external healthcare professional is not required for its placement.
- It is made of silicone, hence it lasts longer
- Can be autoclaved or sanitized easily
- It is made of inert material thus causes no harm to the body
- As it is not placed completely inside the vagina it maintains hygiene and reduces the risk of infection and negligence.
You may also like Best Coccyx Cushions for Tailbone Pain
How to Use Femicushion?
Femicushion can be self-placed and does not require a healthcare provider to provide help. The selection of femicushion is important for the device to provide support and help with the symptoms.
They come in three different sizes and size is selected based on the width of introitus (vaginal opening). The femicushion is then inserted in the vagina and placed on a specific pad which is attached, usually with Velcro, to the support garment/ adjustable underwear.
The accessory garment keeps the femicushion in a correct position and helps in preventing the descend of the device beyond the vaginal introitus(opening).
After the placement, patients are advised to maintain the hygiene of the device. The device is to be worn in the day time and removed at night for cleaning thereby preventing odor, secretion, or infection of the vagina.
Here we have a video demonstration on how to wear Femicushion.
Supporting accessories for Femicushion
- Holder: It is an absorbable, disposable pad placed right on the femicushion. It helps to secrete vaginal discharge and urination and needs to be changed regularly.
- Supporter: It is an adjustable high waist garment used to support the placement of femicushion. It can be easily washed and is reusable.
- Belt- Adjustable straps are are placed on the garment to provide extra support and prevent falling of the device.
- Pillow: Placement of a pillow under the legs like a wedge pillow while lying in a supine position can also be an accessory to provide support to the organs and the device.
How to Clean the Device?
Remove the garments and take out the device from the holder. Dispose of the holder. Insert a cleaning plug at the back of the device. Rinse it under soap and warm water. Air-dry the cushion and place it on a fresh new holder.
You may also like Best Hemorrhoid Pillows
Patient Reviews of Femicushion
Patient surveys after using femicushion daily for three months have shown a positive effect. Improvement in vaginal symptoms especially abdominal pain and descending lump was widely observed. Many were positively able to pass urine normally. A positive impact on life was recorded2.
References:
- Chung, S. H., & Kim, W. B. (2018)
- Souto, Sophia & Palma, Thais & Palma, Paulo, 2016
- Image source – https://commons.wikimedia.org/wiki/File:Uterine_Prolapse.png