Prolapsed bladder and sleep have been associated with each other. Signs and symptoms of prolapse can impact sleep quality, which can lead to a host of other negative consequences for a patient’s health.
Pelvic organ prolapse (POP) is a condition common in women during their child-bearing ages. This may occur due to weakness and stretching of the muscles and ligaments of the pelvic muscles. By not being able to support its position, the pelvis may slip downwards to the opening of the vagina. This can cause bladder weakness and incontinence, and affect a woman’s sexual life and overall physical health.
However, symptoms of prolapsed bladder are treatable, and quality of sleep with prolapsed bladder can be improved if the right sleep routines are adopted.
Contents
Types and Stages of Prolapsed Bladder
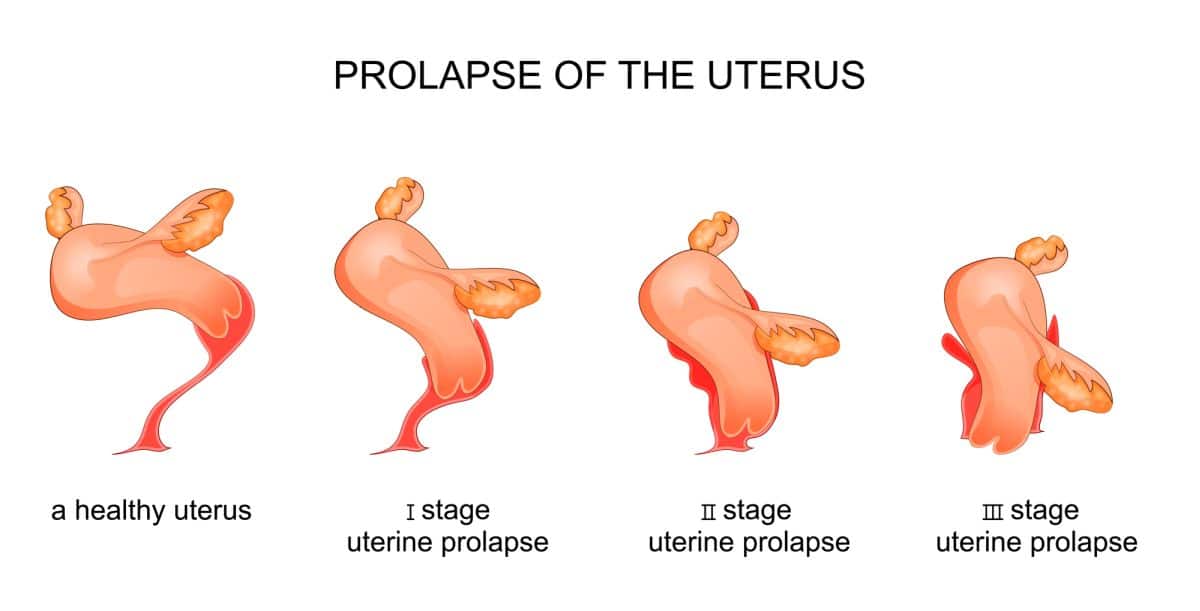
There are four main classifications for types of prolapse. Once identified, one can determine a course of action. This can be possible using the POP-Q system, which talks about describing, staging and quantifying the women pelvic support.
.
Anterior Prolapse
The bladder bulges into the front wall of the vagina. This is also known as a cystocele, the most common prolapse reported in women. Experts estimate that nearly half of women who have given birth experience some degree of pelvic organ prolapse.
The other types for a differential diagnosis include:
Uterine Prolapse
It is described as the uterus falling down towards the vaginal opening. This is further described to be when the womb itself either protrudes or descends out of the vagina. This often affects postmenopausal women who have had one or more vaginal deliveries.
Vagina Vault Prolapse
This is when the vaginal top sags downwards. It is seen in women who have undergone surgery to remove the womb. This usually occurs in women who have had a hysterectomy (removal of the uterus).
About one-third of women will experience some degree of prolapse during their lifetime.
Posterior Vaginal Prolapse
This is also called rectocele. When the separation wall between the rectum and vagina becomes weak, the wall of the vagina bulges out. This can be noticeable as a bulge of tissue at the opening of the vagina. While it may be uncomfortable, it is often not painful.
Stages of Bladder Prolapse
- Grade 1: In this stage, a portion of bladder is seen drooping into vagina – mild stage.
- Grade 2: The bladder droops enough to be able to reach the opening of the vagina – moderate stage.
- Grade 3: The bladder protrudes from the body through the vaginal opening – severe stage.
- Grade 4: This is the case where the total bladder of the vagina protrudes out of the vagina – complete stage.
You may also like Best Weighted Blankets for Insomnia and Restless Legs
Causes of Prolapsed Bladder
The following conditions can cause prolapse.
Pregnancy
Most cases of prolapsed bladder occur as a result of vaginal childbirth delivery. The likelihood of prolapse may increase if the baby was large or delivered quickly, or if there was a prolonged pushing phase.
Having twins or triplets can also cause prolapse. In addition, having multiple pregnancies over time can lead to complete pelvic organ prolapse if signs are left unattended.
Obesity
The risk of prolapse progression in overweight and obese women compared with normal-weight women is increased by 32% and 48% for cystocele, 37% and 58% for rectocele, and 43% and 69% for uterine prolapse. This is caused by increased intra-abdominal pressure, and weakening of the muscles holding the area.
Straining on the toilet to pass a bowel motion
While straining on the toilet can be normal to push feces, excessive straining can trigger hemorrhoids and prolapse. Prolapse can occur with frequent constipation, wherein voiding is difficult.
By forceful voiding, pressure increases on these areas and can also cause hemorrhoids. Proper hydration and intake of fiber can avoid this occurrence.
You may also like Benefits of Sleeping in the Afternoon for the Elderly
Low levels of estrogen after menopause
After menopause, the integrity of muscles, ligaments, and connective tissue weakens. In addition, a reduction in levels of estrogen occurs, and ability to tolerate weight and activity decreases.
This can affect the tissues that hold the uterus in place. Back, hip, and pelvis pain are the common complaints in older women.
Severe Coughing
Severe coughing can be associated with conditions such as chronic bronchitis or asthma fibroids. In order to cough, expiratory muscles of the abdomen forcefully contract.
Chronic cough can exacerbate intra-abdominal pressure, which affects the muscles, ligaments, and connective tissue holding the pelvis.
Pelvic tumor
In rare cases, prolapse can occur when there is a growing tumor in the area of the pelvis. Vaginal, endometrial, and colorectal cancer are the common case studies.
Further studies are still in development to determine the validity of association with cancer. Consulting your oncologist is the best way to confirm any complications associated with your condition.
You may also like How to Sleep With Lower Back Pain and Sciatica?
Signs and Symptoms of Prolapsed Bladder
The common signs and symptoms of prolapsed bladder vary with different diagnoses of the types and stages. POP-Q serves as a guideline that physicians follow.
Most women complain of pressure and discomfort when they have sex or do any physical activity. This also varies by time of day and may be further perpetuated by standing for long periods of time. Other symptoms are as follows:
- When you feel or see something you of the vagina. Protruding of tissue can be felt on the vaginal opening.
- Discomfort, fullness, pressure, and aching in the pelvic region.
- Increased pressure in the pelvis while coughing or standing.
- Leaking urine (incontinence) or problems when you have a bowel movement.
- Problems inserting tampons.
- Inability to empty bladder, or a frequent urge without being able to pass much urine.
- Rare cases may involve urinary tract infections.
There is a high prevalence of sleep disturbance in women seeking care for pelvic organ prolapse. Women with POP have reported that their symptoms of incontinence and pain have led to disturbances in their sleep quality. Young and pre-menopausal women are the common patients that are complaining about this matter.
Prolapsed Bladder Treatment
For as long it is not affecting day-to-day life, there is no need for treatment. However, if symptoms do not go away, medical attention is needed.
Relevant treatment will depend on the stage or level of bladder prolapse. Individuals with mild cases are advised to do kegel exercises along with lifestyle changes. Those with moderate cases will opt for the same approach with the option of a pessary. Severe cases may opt for surgery.
You may also like Femicushion for Prolapse
Kegel Exercises (Pelvic Floor Exercises)
Those with mild to moderate cases may benefit from doing kegel exercises. This will help strengthen pelvic floor muscles and relieve pain. People who are unable to hold their bladder (stress incontinence) or who feel pressure in their abdomen can do this exercise. Please see the following link for exercises to follow.
Pessary
In some cases, a prosthesis called a pessary is inserted into the vagina to support the internal structure of the pelvis. A support pessary or a space-filling pessary may be used depending on the individual case. Not everyone opts for this treatment due to potential discomfort.
Surgery
The surgical repair of bladder prolapse is possible through an incision in the abdomen. Repair in the urethra and bladder can be done by making an incision in the vaginal wall. This method pulls together the loose or torn tissue in the area of prolapse in the bladder or urethra and strengthens the wall of the vagina.
You may also like Wedge Pillow for Prolapse – How to Sleep With a Prolapsed Bladder or Disc
Sleeping Positions and Precautions
When sleeping with a prolapsed bladder, the way you sleep will have an impact on the position of pelvic organ.
Lying in a supported supine position or on the back is comfortable for most patients. When lying in the supine position, place one pillow under the knees. This will help in reliving the pressure from the back and allows you to do ankle pumps.
You can also lay on your side with support, as this is another common sleeping position. If it is comfortable for you, place a pillow between your legs when laying on your side. This can prevent misplacing your pelvis unconsciously when sleeping, and keep your hips aligned.
Use one appropriate-sized bed pillow to support your head and neck in a neutral position. It is not appropriate to use two large pillows on your head and neck. This will cause strain on your neck, and even on the upper back.
You can also avoid sitting for long periods of time unless medically advised.
Precautions
It is recommended to not do forceful activities when diagnosed with POP. This can trigger pressure on your pelvis and can aggravate your symptoms.
It is also advised not to go for long walks and sit for long periods of time. Change your body positions frequently and do light activities like pelvic exercises to strengthen your pelvis and help tolerate changes in your body.
Unless you are medically advised, avoid sitting upright for long periods. In general, avoid positions that can cause you pain.
One-third of women will experience POP once in their life, either from pregnancy, childbirth, menopause, or even a chronic cough. Consult your doctor if you experience the symptoms mentioned above.
Avoid straining on bowel movements, constipation, and smoking. Also, maintain a healthy weight to be fit and reduce the risk of developing POP.