When it comes to Fibromyalgia syndrome, or FMS, the trickiest part for any individual is ascertaining if indeed they do suffer from the condition.
Because FMS is such a complicated and still not entirely understood illness, there is no easy diagnostic process. The term fibromyalgia is derived from the Latin word for fibrous tissue (fibro) and the Greek words for muscle (myo) and pain (algia).
Unlike many other illnesses, there are no laboratory tests or foolproof methods of actually diagnosing FMS. Unfortunately, this means that many sufferers go for years without having the syndrome being successfully diagnosed.
Often doctors will make several other diagnoses beforehand – and this is quite a common trajectory as FMS symptoms mimic several other illnesses.

The Correct Way to Diagnose Fibromyalgia: A Clear and Knowledgeable Guide
Diagnosing fibromyalgia can be a challenging task for doctors as there are no specific laboratory tests or imaging studies to confirm the diagnosis. Instead, doctors rely on physical exams and patient’s symptoms to make a diagnosis.
The American College of Rheumatology (ACR) has established criteria for the diagnosis of fibromyalgia, which include widespread pain in all four quadrants of the body for at least three months, and the presence of at least 11 out of 18 tender points on physical examination.
In addition to the physical exam, doctors may also order blood tests to rule out other conditions that may have similar symptoms. These tests may include a complete blood count (CBC), erythrocyte sedimentation rate (ESR), and celiac serology.
To assess the severity of fibromyalgia symptoms, doctors may use a symptom severity scale, which includes questions about pain, fatigue, sleep, and mood. The score on this scale can help doctors track the progress of the disease and evaluate the effectiveness of treatment.
It is important to note that a normal blood test result does not rule out fibromyalgia, and not all patients with fibromyalgia will have tender points on physical examination. Therefore, doctors must rely on a combination of patient’s symptoms and physical exam findings to make a diagnosis of fibromyalgia.
The tender point examination system
There are two systems of diagnosing FMS, with the tender point examination having been heavily criticised in recent years.
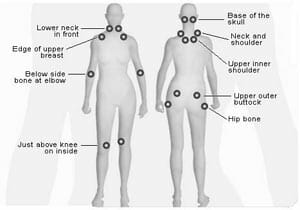
Derived in 1990 by the American College of Rheumatology, this examination makes use of a system of 18 tender points on the body which are particularly sensitive to pressure. These are localised areas of pain located near joints which often become inflamed.
For a diagnosis of FMS to be made, 11 of 18 tender points must be painful when pressed (see illustration).
While this method has had varying results, some claim that it is only 75% effective in detecting FMS, mostly because pain levels can fluctuate greatly on a day to day basis.
Usually such a diagnosis will need to be made by a rheumatologist who will test each of the paired tender points. Nowadays, however, even neurologists are branching out in the treating FMS.
New diagnostic criteria
Since 2010, a newer system of diagnosing FMS has emerged. This system does away with tender point examinations and instead makes use of a widespread pain index coupled with a symptom severity scale.
The widespread pain index is a list of 19 different areas on the body, where the patient may have experienced pain in the last week.
For each area where pain has been experienced, you assign a score of 1 point, with a possible total of 19 points should you have experienced pain in every area. These areas are as follows:
- Shoulder girdle, left
- Shoulder girdle, right
- Upper arm left
- Upper arm right
- Hip (buttock, trochanter) left
- Hip (buttock, trochanter), right
- Jaw, left
- Jaw, right
- Upper back
- Lower back
- Upper leg, left
- Upper leg, right
- Neck
- Chest
- Abdomen
- Lower arm, left
- Lower arm, right
- Lower leg, left
- Lower leg, right
For symptom severity, the patient assigns a score of 0 to 3 to the following possible symptoms:
- Fatigue
- Unrefreshing sleep
- Cognitive disruption or problems
- Somatic symptoms in general (these include headaches, physical weakness, irritable bowel syndrome, bladder/urination issues, nausea, dizziness, numbness/tingling or hair loss)
The totals of the severity symptoms are then added up with a possible maximum of 12 points, where 0 = no problem, 1 = slight or mild problems, generally mild or intermittent, 2 = moderate, considerable problems, often present and/or at a moderate level, and 3 = severe: pervasive, continuous, life-disturbing problems.
Finally, your doctor can compare your scores on both lists to determine your possibility of FMS. For a diagnosis of FMS, you need to score at least a 7 on the widespread pain index AND at least a 5 on the severity symptom scale.
Alternatively, you could also score between 3 and 6 on the widespread pain index AND at least a 9 on the symptom severity scale.
Medical Specialists for Fibromyalgia
When it comes to diagnosing fibromyalgia, there are several medical specialists who can help. Here are some of the most common specialists who may be involved in the diagnosis and treatment of fibromyalgia:
Rheumatologists
Rheumatologists are medical doctors who specialize in diagnosing and treating conditions that affect the joints, muscles, and bones. They are often the first specialists to be consulted when someone is experiencing widespread pain and other symptoms associated with fibromyalgia. Rheumatologists can perform a physical exam, order lab tests, and recommend imaging studies to help diagnose fibromyalgia.
Exercise Physiologists
Exercise physiologists specialize in developing exercise programs for people with chronic conditions, including fibromyalgia. They can help patients improve their physical fitness, reduce pain, and increase their overall quality of life. Exercise physiologists may work in a variety of settings, including hospitals, rehabilitation centers, and private clinics.
Mental Health Professionals
Mental health professionals, such as psychologists and psychiatrists, can play an important role in the diagnosis and treatment of fibromyalgia. They can help patients manage the emotional and psychological aspects of the condition, such as depression, anxiety, and stress. Mental health professionals may use a variety of techniques, such as cognitive-behavioral therapy, to help patients cope with fibromyalgia.
Pain Management Specialists
Pain management specialists are medical doctors who specialize in treating chronic pain conditions, such as fibromyalgia. They can prescribe medications, such as pain relievers and muscle relaxants, and recommend other treatments, such as physical therapy and acupuncture. Pain management specialists may work in a variety of settings, including hospitals, clinics, and private practices.
Physical Therapists
Physical therapists specialize in helping patients improve their physical function and mobility. They can develop exercise programs and other treatments to help patients with fibromyalgia manage their symptoms. Physical therapists may work in a variety of settings, including hospitals, rehabilitation centers, and private clinics.
Primary Health Care Providers
Primary health care providers, such as family doctors and nurse practitioners, can play an important role in the diagnosis and treatment of fibromyalgia. They can perform a physical exam, order lab tests, and recommend imaging studies to help diagnose the condition. They can also prescribe medications and recommend other treatments, such as physical therapy and exercise.
Sleep Specialists
Sleep specialists are medical doctors who specialize in diagnosing and treating sleep disorders, such as sleep apnea and insomnia. They can help patients with fibromyalgia manage their sleep problems, which are often a major symptom of the condition. Sleep specialists may work in a variety of settings, including hospitals, clinics, and private practices.

Research and Clinical Trials
Research and clinical trials have been conducted to improve the diagnosis of fibromyalgia. These studies aim to develop reliable diagnostic criteria and identify biomarkers that can help detect the condition.
One study published in the Journal of Rheumatology found that a combination of tender point count and the widespread pain index can accurately diagnose fibromyalgia. The study involved 829 patients with fibromyalgia and 1,640 control subjects. The researchers found that this diagnostic approach had a sensitivity of 88.4% and a specificity of 81.1%.
Another study published in the Journal of Clinical Rheumatology evaluated the effectiveness of a new diagnostic tool called the Fibromyalgia Rapid Screening Tool (FiRST). The tool includes a questionnaire and a physical examination. The study involved 150 patients with fibromyalgia and 150 control subjects. The researchers found that the tool had a sensitivity of 92% and a specificity of 86%.
Clinical trials have also been conducted to evaluate the effectiveness of various treatments for fibromyalgia. One such trial published in the Journal of Pain Research evaluated the effectiveness of acupuncture for fibromyalgia. The trial involved 100 patients with fibromyalgia who received either true acupuncture or sham acupuncture. The researchers found that true acupuncture was significantly more effective than sham acupuncture in reducing pain and improving quality of life.
Overall, research and clinical trials have provided valuable insights into the diagnosis and treatment of fibromyalgia. While more research is needed, these studies have helped improve the accuracy of diagnosis and identify effective treatments for this condition.
Differential Diagnoses
When diagnosing fibromyalgia, it is important to consider other conditions that may present with similar symptoms. The following entities are among the most common differential diagnoses:
Irritable Bowel Syndrome (IBS)
IBS is a chronic gastrointestinal disorder characterized by abdominal pain, bloating, and changes in bowel habits. It is often associated with fibromyalgia, and the two conditions can exacerbate each other. Patients with IBS may also experience fatigue and sleep disturbances, which can make it difficult to differentiate between the two conditions. However, IBS can be diagnosed through a combination of symptoms and diagnostic tests, such as stool analysis and colonoscopy.
Sleep Apnea
Sleep apnea is a condition in which a person’s breathing is interrupted during sleep, leading to daytime fatigue and other symptoms. It is often associated with fibromyalgia, as both conditions can cause sleep disturbances. However, sleep apnea can be diagnosed through a sleep study, which measures the patient’s breathing patterns and oxygen levels during sleep.
Lyme Disease
Lyme disease is a bacterial infection that is transmitted through the bite of an infected tick. It can cause a wide range of symptoms, including fatigue, joint pain, and muscle aches, which can be similar to those of fibromyalgia. However, Lyme disease can be diagnosed through blood tests that detect antibodies to the bacteria.
Spine Conditions
Spine conditions, such as herniated discs and spinal stenosis, can cause chronic pain and other symptoms that may be mistaken for fibromyalgia. However, these conditions can often be diagnosed through imaging tests, such as MRI or CT scans.
In conclusion, while fibromyalgia can be difficult to diagnose, it is important to consider other conditions that may present with similar symptoms. By ruling out other possible causes, healthcare providers can ensure that patients receive the most appropriate treatment for their condition.

Sure I have it, had it after a knee surgery. That triggered it.
Along with osteoporosis, arthritis,DDD,spondythothisis,venious insufficiently, just to name a few. Have been on pain meds since. Now that the government has gotten involved. They are taking all my meds away. And I get to be in pain every day. Not to mention fighting for social security for 5 years. Which I had to give up. We were going to have to live on the streets if I didn’t go to work.
The only way I can function at work is with my meds. I’m so scared of what is going to happen without them. They have already started the prices of cutting my meds. My depression has gotten worse.
Sure I have it, had it after a knee surgery. That triggered it.
Along with osteoporosis, arthritis,DDD,spondythothisis,venious insufficiently, just to name a few. Have been on pain meds since. Now that the government has gotten involved. They are taking all my meds away. And I get to be in pain every day. Not to mention fighting for social security for 5 years. Which I had to give up. We were going to have to live on the streets if I didn’t go to work.
The only way I can function at work is with my meds. I’m so scared of what is going to happen without them. They have already started the prices of cutting my meds. My depression has gotten worse.
Mainey, I feel your pain. There is a hysteria going on about the use of Opioids. The AMA has made it clear that doctors are over prescribing and Dr.s who don’t have the guts to fight for their patients are just yanking this stuff off the market, even after major surgery!! If a dr is monitoring your usage and it is medically necessary and you are not addicted, I feel it is inhumane!!
Mainey, I feel your pain. There is a hysteria going on about the use of Opioids. The AMA has made it clear that doctors are over prescribing and Dr.s who don’t have the guts to fight for their patients are just yanking this stuff off the market, even after major surgery!! If a dr is monitoring your usage and it is medically necessary and you are not addicted, I feel it is inhumane!!
The excuse the government gives in restricting opiods is people either get addicted and eventually have to buy their drugs on the streets or some people overdose on them. Well guess what, they are doing the opposite of what they want to accomplish. They are going to drive people to the street to get their meds and instead of overdosing on them, people will commit suicide if they can’t get relief from their pain. I would like to see the people who are making these be in my kind of pain and give them either a low dose of pain med or no pain meds.
The excuse the government gives in restricting opiods is people either get addicted and eventually have to buy their drugs on the streets or some people overdose on them. Well guess what, they are doing the opposite of what they want to accomplish. They are going to drive people to the street to get their meds and instead of overdosing on them, people will commit suicide if they can’t get relief from their pain. I would like to see the people who are making these be in my kind of pain and give them either a low dose of pain med or no pain meds.